1 Section on Medical Neuroendocrinology, Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, Bethesda, Maryland.
Search for other works by this author on: David Taïeb2 Department of Nuclear Medicine, La Timone University Hospital, CERIMED, Aix-Marseille University, Marseille, France.
Search for other works by this author on: Jorge A. Carrasquillo3 Department of Radiology, Molecular Imaging and Therapy Service, Memorial Sloan Kettering Cancer Center, New York, New York.
4 Department of Radiology, Weill Cornell Medical College, New York, New York. Search for other works by this author on: Daniel A. Pryma5 Department of Radiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, Pennsylvania.
Search for other works by this author on: Mayank Patel1 Section on Medical Neuroendocrinology, Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, Bethesda, Maryland.
Search for other works by this author on: Corina Millo6 Department of Positron Emission Tomography, Warren Grant Magnuson Clinical Center, National Institutes of Health, Bethesda, Maryland.
Search for other works by this author on: Wouter W. de Herder7 Section of Endocrinology, Department of Internal Medicine, ENETS Centre of Excellence, Erasmus MC Cancer Institute, Erasmus MC, Rotterdam, the Netherlands.
Search for other works by this author on: Jaydira Del Rivero 8 Developmental Therapeutics Branch, Center for Cancer Research, NCI, NIH, Bethesda, Maryland. Search for other works by this author on: Joakim Crona 9 Department of Medical Sciences, Uppsala University, Uppsala, Sweden. Search for other works by this author on: Barry L. Shulkin 10 Department of Diagnostic Imaging, St. Jude Children's Research Hospital, Memphis, Tennessee. Search for other works by this author on: Irene Virgolini 11 Department of Nuclear Medicine, Medical University of Innsbruck, Innsbruck, Austria. Search for other works by this author on: Alice P. Chen 12 Division of Cancer Treatment and Diagnosis, NCI, NIH, Bethesda, Maryland. Search for other works by this author on: Bhagwant R. Mittal13 Department of Nuclear Medicine, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
Search for other works by this author on: Sandip Basu14 Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Hospital Annexe, Homi Bhabha National Institute, Mumbai, Maharashtra, India.
Search for other works by this author on: Joseph S. Dillon 15 Department of Internal Medicine, University of Iowa Hospitals and Clinics, Iowa City, Iowa. Search for other works by this author on: Thomas A. Hope16 Department of Radiology and Biomedical Imaging, University of California, San Francisco, California.
Search for other works by this author on: Carina Mari Aparici17 Divisions of Nuclear Medicine and Molecular Imaging, Stanford University School of Medicine, Stanford, California.
Search for other works by this author on: Andrei H. Iagaru17 Divisions of Nuclear Medicine and Molecular Imaging, Stanford University School of Medicine, Stanford, California.
Search for other works by this author on: Rodney J. Hicks18 Sir Peter MacCallum Department of Oncology, University of Melbourne, Melbourne, Victoria, Australia.
Search for other works by this author on: Anca M. Avram19 Division of Nuclear Medicine, Department of Radiology, University of Michigan, Ann Arbor, Michigan.
Search for other works by this author on: Jonathan R. Strosberg20 Division of Neuroendocrine Tumor/Department of Gastrointestinal Medicine, Moffitt Cancer Center, Tampa, Florida.
Search for other works by this author on: Ali Cahid Civelek21 Division of Nuclear Medicine and Molecular Imaging, Department of Radiology and Radiological Sciences, Johns Hopkins Medicine, Baltimore, Maryland.
Search for other works by this author on: Frank I. Lin 22 Molecular Imaging Program, NCI, NIH, Bethesda, Maryland. Search for other works by this author on: Neeta Pandit-Taskar *3 Department of Radiology, Molecular Imaging and Therapy Service, Memorial Sloan Kettering Cancer Center, New York, New York.
4 Department of Radiology, Weill Cornell Medical College, New York, New York. Search for other works by this author on: Karel Pacak *1 Section on Medical Neuroendocrinology, Eunice Kennedy Shriver National Institute of Child Health and Human Development, NIH, Bethesda, Maryland.
Search for other works by this author on:N. Pandit-Taskar and K. Pacak contributed equally to this article.
Clin Cancer Res 2021;27:2989–95
Received: September 18 2020 Revision Received: November 14 2020 Accepted: March 03 2021 Online ISSN: 1557-3265 Print ISSN: 1078-0432 Award Group: National Institute of Child Health and Human Development Award Group: P30 CA008748 ©2021 American Association for Cancer Research. American Association for Cancer Research. Clin Cancer Res (2021) 27 (11): 2989–2995. September 18 2020 Revision Received: November 14 2020 March 03 2021Abhishek Jha , David Taïeb , Jorge A. Carrasquillo , Daniel A. Pryma , Mayank Patel , Corina Millo , Wouter W. de Herder , Jaydira Del Rivero , Joakim Crona , Barry L. Shulkin , Irene Virgolini , Alice P. Chen , Bhagwant R. Mittal , Sandip Basu , Joseph S. Dillon , Thomas A. Hope , Carina Mari Aparici , Andrei H. Iagaru , Rodney J. Hicks , Anca M. Avram , Jonathan R. Strosberg , Ali Cahid Civelek , Frank I. Lin , Neeta Pandit-Taskar , Karel Pacak; High-Specific-Activity- 131 I-MIBG versus 177 Lu-DOTATATE Targeted Radionuclide Therapy for Metastatic Pheochromocytoma and Paraganglioma. Clin Cancer Res 1 June 2021; 27 (11): 2989–2995. https://doi.org/10.1158/1078-0432.CCR-20-3703
Download citation file:
toolbar searchTargeted radionuclide therapies (TRT) using 131 I-metaiodobenzylguanidine ( 131 I-MIBG) and peptide receptor radionuclide therapy ( 177 Lu or 90 Y) represent several of the therapeutic options in the management of metastatic/inoperable pheochromocytoma/paraganglioma. Recently, high-specific-activity- 131 I-MIBG therapy was approved by the FDA and both 177 Lu-DOTATATE and 131 I-MIBG therapy were recommended by the National Comprehensive Cancer Network guidelines for the treatment of metastatic pheochromocytoma/paraganglioma. However, a clinical dilemma often arises in the selection of TRT, especially when a patient can be treated with either type of therapy based on eligibility by MIBG and somatostatin receptor imaging. To address this problem, we assembled a group of international experts, including oncologists, endocrinologists, and nuclear medicine physicians, with substantial experience in treating neuroendocrine tumors with TRTs to develop consensus and provide expert recommendations and perspectives on how to select between these two therapeutic options for metastatic/inoperable pheochromocytoma/paraganglioma. This article aims to summarize the survival outcomes of the available TRTs; discuss personalized treatment strategies based on functional imaging scans; address practical issues, including regulatory approvals; and compare toxicities and risk factors across treatments. Furthermore, it discusses the emerging TRTs.
Translational RelevanceClinical decision-making in the selection of appropriate targeted radiotherapy [ 131 I-metaiodobenzylguanidine ( 131 I-MIBG) and peptide receptor radionuclide therapy (PRRT; 177 Lu/ 90 Y)] for patients is a clinical dilemma. The decision should be personalized on the basis of the clinical presentation and MIBG and somatostatin receptor imaging. The agent that shows greater tumor targeting with more favorable toxicity profile and associated risk factors should be chosen for therapy. Heterogeneous disease with mismatched MIBG and somatostatin receptor avid lesions, possess additional challenge in decision-making regarding choice of therapeutic agent. A combined or sequential regimen can be considered in such a situation. Additional external beam radiation for targeting any progressive lesions lacking uptake by both of the imaging modalities should be considered. Our perspective based on expert opinion and consensus provides a stepwise approach to selection of targeted systemic radiotherapy for patients with metastatic/inoperable pheochromocytoma/paraganglioma. In patients with large-sized or variable-sized tumors, 90 Y-based PRRT alone or in combinations (tandem or duo approaches) with other targeted radiotherapies can be entertained.
Targeted radionuclide therapies (TRT) using 131 I-metaiodobenzylguanidine ( 131 I-MIBG) and peptide receptor radionuclide therapy (PRRT; 177 Lu or 90 Y) are available for metastatic/inoperable pheochromocytoma/paraganglioma. It is unclear which therapy is preferable when tumors show uptake by both MIBG [generally 123 I-MIBG single-photon emission CT/CT (SPECT/CT), but potentially also 124 I-MIBG or 18 F-metafluorobenzylguanidine ( 18 F-MFBG) or 18 F-fluorodopamine ( 18 F-FDA) PET/CT] and somatostatin receptor imaging (SSTRI; 111 In-pentetreotide or 68 Ga-DOTA-TATE/TOC/NOC PET/CT or 64 Cu-DOTATATE PET/CT). 131 I-MIBG is a safe and well-tolerated therapy, used since the 1980s with objective, biochemical, and symptomatic responses in patients with paraganglioma (1). The recent FDA approval of novel high-specific-activity (HSA)- 131 I-MIBG therapy (Azedra®; Progenics Pharmaceuticals, Inc.) in metastatic/inoperable pheochromocytoma/paraganglioma has generated considerable interest (2). Similarly, the recent FDA approval of 177 Lu-DOTATATE (Lutathera®; Advanced Accelerator Applications USA, Inc., a Novartis company) for gastroenteropancreatic neuroendocrine tumors (GEP-NET) has led to an increasing interest in its use for other SSTR-expressing NETs, including pheochromocytomas/paragangliomas (3–6). Availability of both of these TRTs presents a conundrum regarding the selection of the most appropriate option in patients who are candidates for TRTs. Therefore, we assembled experts in the field of oncology, endocrinology, and nuclear medicine to develop consensus and provide an expert opinion on how to select between these two therapeutic options for metastatic/inoperable pheochromocytoma/paraganglioma.
Recently, an HSA formulation consisting almost entirely of radiolabeled 131 I-MIBG (∼2,500 mCi/mg) was developed for norepinephrine transporter–expressing tumors resulting in fewer pharmacologic (side) effects than lower specificity formulations of 131 I-MIBG (15–50 mCi/mg), in which only approximately 1:2,000 MIBG molecules have 131 I (2, 7).
HSA- 131 I-MIBG is administered in patients with pheochromocytoma/paraganglioma with positive MIBG scans and either progressive or symptomatic metastatic/inoperable disease. The main therapeutic goals are disease stabilization and symptom control. Treatment is given following dosimetry assessment using HSA- 131 I-MIBG imaging over 3–5 days. A standard treatment regimen consists of two doses of 500 mCi (or 8 mCi/kg if weight
In a single-arm phase II trial, 68 patients with metastatic/inoperable pheochromocytoma/paraganglioma were treated with up to two cycles of HSA- 131 I-MIBG. The primary endpoint, reduction in baseline antihypertensive medication lasting ≥6 months, was reached in 25% of patients (2). Furthermore, an objective partial response (PR; 23%) or stable disease (SD; 69%) within 12 months was seen in 92% of patients by RECIST 1.0; 68% showed complete response (CR) or PR in serum chromogranin levels. The median overall survival (OS) was 36.7 months from the first treatment (2). Moreover, the PR rate increased from 6% at 3 months to 23% at 12 months among patients receiving at least one therapeutic dose, indicating that HSA- 131 I-MIBG effects can evolve over many months (2).
The most common side effects were myelosuppression, nausea/vomiting, and fatigue (2). A total of 72% (49/68) of patients in the phase II HSA- 131 I-MIBG trial experienced grade ≥3 hematotoxicity (41% thrombocytopenia, 41% leukopenia, 38% neutropenia, and 21% anemia) and 25% (17/68) required hematologic supportive care (packed red blood cells, platelets, colony-stimulating factors, and/or erythropoietin-alfa therapy for limited time; ref. 2). Other severe adverse events included pulmonary embolism in 3% (2/68), myelodysplastic syndrome in 4% (3/68), and secondary malignancies in 3% (acute myeloid leukemia and acute lymphocytic leukemia in 1 patient each; ref. 2). Less common side effects included headache, dizziness, and fatigue (16%–27%; ref. 2). No acute hypertensive event was noted during or after the administration of HSA- 131 I-MIBG. Similarly, nephrotoxicity was not reported (2). Of note, some patients in this phase II trial were pretreated, with most having received at least one prior cytotoxic systemic therapy (38% chemotherapy and 30% 131 I-MIBG and/or HSA- 131 I-MIBG TRT) and few having received several prior lines of cytotoxic systemic therapies (2).
PRRT with 177 Lu-DOTATATE was FDA approved in 2018 for patients with well-differentiated metastatic/inoperable GEP-NETs following favorable progression-free survival (PFS) and quality-of-life outcomes in a phase III study of patients with progressing midgut NETs and the results of ongoing studies in the Erasmus MC (Rotterdam, the Netherlands; refs. 3, 8, 9). 177 Lu-DOTATATE has been used to treat patients with metastatic/inoperable pheochromocytoma/paraganglioma, although the published data are limited to small uncontrolled retrospective studies using various dose regimens and radiopharmaceuticals ( 177 Lu/ 90 Y-DOTATATE/DOTATOC; refs. 5, 6). In a meta-analysis of 179 pooled patients treated with 1–11 cycles of PRRT ( 90 Y and/or 177 Lu), 90% [95% confidence interval (CI), 84%–95%] had achieved PR or SD (5). Similarly, a meta-analysis performed by Satapathy and colleagues reported an objective response rate [proportion of CR, PR, and/or minor response (MR)] of 25% (95% CI, 19%–32%) and a disease control rate (proportion of CR, PR, MR, and SD) of 84% (95% CI, 77%–89%) in 201 pooled patients (progressive disease
PRRT is usually administered in fixed dose cycles of 200 mCi/cycle of 177 Lu-DOTATATE infusion over 30–60 minutes with concomitant amino acid infusion for renal protection. Because of fixed dose therapy, dosimetry preparation/estimation is not routinely performed. Some centers have used dosimetric estimates, primarily to limit renal dose to 23 Gray and bone marrow to 2 Gray (11). Renal protection is provided by concomitant amino acid infusion. Some currently available commercial preparations contain many different amino acids, which have a high rate of associated nausea and/or vomiting even with administration of antiemetics, but the incidence can be substantially reduced by using a preparation that includes only L-lysine and L-arginine.
On the basis of its regulatory approval and commercial availability, 177 Lu-DOTATATE has displaced 90 Y-DOTATOC in recent years. Moreover, 177 Lu has longer half-life and gamma emission, which also allows for imaging both for dosimetry, if desired, and post-therapy assessment (Table 1). A meta-analysis in pheochromocytoma/paraganglioma reported a pooled grade 3/4 thrombocytopenia, neutropenia, and lymphopenia in 9%, 3%, and 11% of the treated patients, respectively, and nephrotoxicity in 4% of patients (6). The therapy was discontinued for toxicity in only 4.9% (5/102) of patients (6). Reversible cardiac failure following catecholamine release (6.7%) and myelodysplastic syndrome (3.3%) has also been reported following 177 Lu-DOTATATE therapy (12). Furthermore, development of catecholamine crises and tumor lysis syndrome was also observed following 177 Lu-DOTATATE (13).
Targeted radiotherapies in pheochromocytoma/paraganglioma.
Abbreviation: EMA, European Medicines Agency.
a 90 Y-based PRRT can be an alternative to 177 Lu-DOTATATE in certain cases.
c Awarded orphan drug status for 90 Y-edotreotide between 2008 and 2018 by the EMA (https://www.ema.europa.eu/en/medicines/human/orphan-designations/eu308589).
d Calculated as a total of two cycles of 500 mCi of HSA- 131 I-MIBG and four cycles of 200 mCi of 177 Lu-DOTATATE.
e Lower (∼$15,000) in centers which synthesize it in-house.
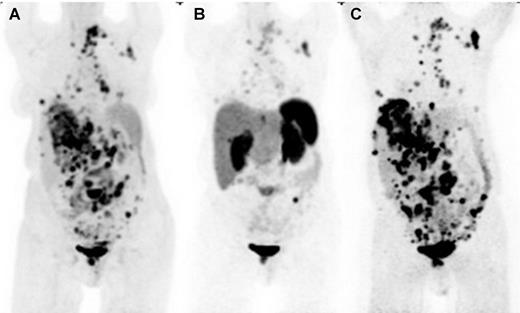
When a patient with metastatic/inoperable pheochromocytoma/paraganglioma presents to the clinic for the evaluation of TRT, the first and foremost step is to consider whether systemic therapy is indicated on the basis of several factors: the disease course (progression vs. SD), catecholamine/metanephrine secretion and related symptoms (e.g., controlled vs. uncontrolled hypertension, arrhythmia, cardiovascular events, and psychiatric symptoms), tumor location, and risk for complications (e.g., neurologic toxicity from vertebral metastases). Consideration of these factors is necessary because some patients with metastatic pheochromocytoma/paraganglioma have indolent disease and are often safely followed with active surveillance and medical management of catecholamine excess (14–16). If the patient is potentially eligible for systemic therapy, particularly TRT, the second step is to evaluate MIBG and SSTRI scans to determine the degree and extent of uptake. It is of prime importance to ensure that the tumors can be targeted by TRT at a whole-body level by comparison of uptake in target lesions with total tumor burden noted on CT/MRI and/or 18 F-fluorodeoxyglucose ( 18 F-FDG) PET/CT (Fig. 1).
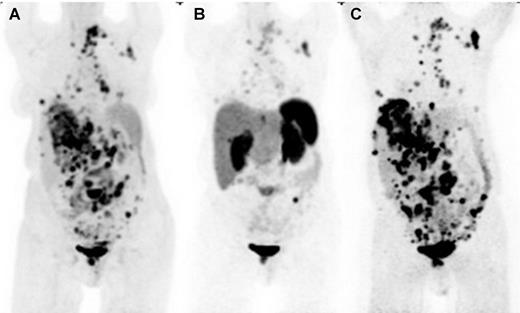
Selection of HSA- 131 I-MIBG over PRRT for metastatic paraganglioma based on superior norepinephrine transporter expression imaged by 124 I-MIBG PET/CT and compared with 18 F-FDG PET/CT. The anterior maximum intensity projection images of 18 F-FDG PET-CT(A), SSTRI by 68 Ga-DOTATATE PET/CT (B), and norepinephrine transporter imaging by 124 I-MIBG PET/CT (C) in a case of widely metastatic paraganglioma. 124 I-MIBG demonstrates more disease sites than 18 F-FDG, as well as has significantly more intense and numerous lesion uptake than 68 Ga-DOTATATE, making MIBG therapy the preferred option for treatment in this case. Advantages of comparing PET ( 68 Ga-DOTATATE) with PET ( 124 I-MIBG) and ability to do prospective dosimetry are potential advantages of 124 I-MIBG over 123 I-MIBG, although this technique is not widely available.
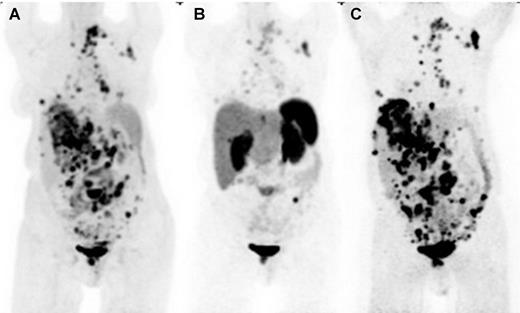
Selection of HSA- 131 I-MIBG over PRRT for metastatic paraganglioma based on superior norepinephrine transporter expression imaged by 124 I-MIBG PET/CT and compared with 18 F-FDG PET/CT. The anterior maximum intensity projection images of 18 F-FDG PET-CT(A), SSTRI by 68 Ga-DOTATATE PET/CT (B), and norepinephrine transporter imaging by 124 I-MIBG PET/CT (C) in a case of widely metastatic paraganglioma. 124 I-MIBG demonstrates more disease sites than 18 F-FDG, as well as has significantly more intense and numerous lesion uptake than 68 Ga-DOTATATE, making MIBG therapy the preferred option for treatment in this case. Advantages of comparing PET ( 68 Ga-DOTATATE) with PET ( 124 I-MIBG) and ability to do prospective dosimetry are potential advantages of 124 I-MIBG over 123 I-MIBG, although this technique is not widely available.
The choice between 131 I-MIBG and 177 Lu-DOTATATE in many cases becomes obvious when lack of uptake is observed with one radiopharmaceutical and not the other, as is frequently seen (Fig. 2A and B). The most important conundrum occurs when both 123 I-MIBG and SSTRI scans demonstrate similar uptake and extent of disease (Fig. 2C).
![Figure 2. Selection of HSA-131I-MIBG versus PRRT for metastatic pheochromocytoma/paraganglioma based on expression of somatostatin receptor and norepinephrine transporter. A, Superior detection of tumors by norepinephrine transporter imaging by 123I-MIBG (anterior and posterior planar images on the right) compared with SSTRI by 68Ga-DOTATATE PET/CT [maximum intensity projection (MIP) image on the left] in a 64-year-old man revealing a recurrent tumor in the left adrenalectomy bed along with retroperitoneal lesions, left supraclavicular lymph node, and multiple scattered bony metastatic disease, including cervical bone metastasis. B, Superior detection of tumors by 68Ga-DOTATATE PET/CT (MIP image on the left) compared with 123I-MIBG (anterior and posterior planar images on the right) in a 33-year-old woman revealing an extensive recurrent tumor in the right adrenalectomy bed at the level of right mid kidney along with metastatic disease in both lungs, scattered bone metastases in vertebral bodies, axial, and proximal appendicular skeleton. The planar images of 123I-MIBG only reveal mild uptake of recurrent tumor in the right adrenalectomy bed. C, Similar pattern of tumor detection by both 68Ga-DOTATATE PET/CT (MIP image on the left) and 123I-MIBG (anterior and posterior planar images on the right) in a 27-year-old female patient revealing metastatic liver lesions and multiple scattered bony metastatic disease. While interpreting the scans, it is critical to account for the inherent differences between single-photon emission imaging (123I-MIBG scintigraphy) and PET (68Ga-DOTATATE) <a href=](https://aacr.silverchair-cdn.com/aacr/content_public/journal/clincancerres/27/11/10.1158_1078-0432.ccr-20-3703/3/m_2989fig2.jpeg?Expires=1728471578&Signature=DMdtz6wOkGPd9Gi-2AamkpqagGzj~QFCBcJrn5kmXj~HKPvxU3Kj681eW8VNKO4VblK2VaHbb9JpPhsZlk39xO5p84cCLuFoPmZouWC2QLSSR61306LNcAekSjUhubJoPdHB1D3Wu9imM9~fUUv8u9uNKueggGCELY6lkAzE6j-OM~se26FAGn4ksHLTViBoe~9qA80pUK75w237n5AVA3aQfzPJ3PpGDJgnJg~IZfmU3wZA6F0KFxQAGIPdMUELvxg-7e6nRzSdkpzd2~NZTP3FRRu8aen8zz6xWmCd4IMg7Nzrf1HEScrgAyPokH6fOASwPLy794r9Yv9uzjsOQQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA) imaging as contrast recovery, sensitivity, and spatial resolution are far superior for PET imaging. Therefore, some of the smaller lesions seen on 68Ga-DOTATATE MIP may not be visible on planar images of 123I-MIBG scintigraphy, despite adequate MIBG uptake. This should not be confused for greater uptake or a higher likelihood of response to therapy. 124I-MIBG 18F-FDA and 18F-MFBG for PET that are under development should help simplify the comparison between MIBG and SSTRI scans in a given patient." />
imaging as contrast recovery, sensitivity, and spatial resolution are far superior for PET imaging. Therefore, some of the smaller lesions seen on 68Ga-DOTATATE MIP may not be visible on planar images of 123I-MIBG scintigraphy, despite adequate MIBG uptake. This should not be confused for greater uptake or a higher likelihood of response to therapy. 124I-MIBG 18F-FDA and 18F-MFBG for PET that are under development should help simplify the comparison between MIBG and SSTRI scans in a given patient." />
Selection of HSA- 131 I-MIBG versus PRRT for metastatic pheochromocytoma/paraganglioma based on expression of somatostatin receptor and norepinephrine transporter. A, Superior detection of tumors by norepinephrine transporter imaging by 123 I-MIBG (anterior and posterior planar images on the right) compared with SSTRI by 68 Ga-DOTATATE PET/CT [maximum intensity projection (MIP) image on the left] in a 64-year-old man revealing a recurrent tumor in the left adrenalectomy bed along with retroperitoneal lesions, left supraclavicular lymph node, and multiple scattered bony metastatic disease, including cervical bone metastasis. B, Superior detection of tumors by 68 Ga-DOTATATE PET/CT (MIP image on the left) compared with 123 I-MIBG (anterior and posterior planar images on the right) in a 33-year-old woman revealing an extensive recurrent tumor in the right adrenalectomy bed at the level of right mid kidney along with metastatic disease in both lungs, scattered bone metastases in vertebral bodies, axial, and proximal appendicular skeleton. The planar images of 123 I-MIBG only reveal mild uptake of recurrent tumor in the right adrenalectomy bed. C, Similar pattern of tumor detection by both 68 Ga-DOTATATE PET/CT (MIP image on the left) and 123 I-MIBG (anterior and posterior planar images on the right) in a 27-year-old female patient revealing metastatic liver lesions and multiple scattered bony metastatic disease. While interpreting the scans, it is critical to account for the inherent differences between single-photon emission imaging ( 123 I-MIBG scintigraphy) and PET ( 68 Ga-DOTATATE) imaging as contrast recovery, sensitivity, and spatial resolution are far superior for PET imaging. Therefore, some of the smaller lesions seen on 68 Ga-DOTATATE MIP may not be visible on planar images of 123 I-MIBG scintigraphy, despite adequate MIBG uptake. This should not be confused for greater uptake or a higher likelihood of response to therapy. 124 I-MIBG 18 F-FDA and 18 F-MFBG for PET that are under development should help simplify the comparison between MIBG and SSTRI scans in a given patient.
![Figure 2. Selection of HSA-131I-MIBG versus PRRT for metastatic pheochromocytoma/paraganglioma based on expression of somatostatin receptor and norepinephrine transporter. A, Superior detection of tumors by norepinephrine transporter imaging by 123I-MIBG (anterior and posterior planar images on the right) compared with SSTRI by 68Ga-DOTATATE PET/CT [maximum intensity projection (MIP) image on the left] in a 64-year-old man revealing a recurrent tumor in the left adrenalectomy bed along with retroperitoneal lesions, left supraclavicular lymph node, and multiple scattered bony metastatic disease, including cervical bone metastasis. B, Superior detection of tumors by 68Ga-DOTATATE PET/CT (MIP image on the left) compared with 123I-MIBG (anterior and posterior planar images on the right) in a 33-year-old woman revealing an extensive recurrent tumor in the right adrenalectomy bed at the level of right mid kidney along with metastatic disease in both lungs, scattered bone metastases in vertebral bodies, axial, and proximal appendicular skeleton. The planar images of 123I-MIBG only reveal mild uptake of recurrent tumor in the right adrenalectomy bed. C, Similar pattern of tumor detection by both 68Ga-DOTATATE PET/CT (MIP image on the left) and 123I-MIBG (anterior and posterior planar images on the right) in a 27-year-old female patient revealing metastatic liver lesions and multiple scattered bony metastatic disease. While interpreting the scans, it is critical to account for the inherent differences between single-photon emission imaging (123I-MIBG scintigraphy) and PET (68Ga-DOTATATE) <a href=](https://aacr.silverchair-cdn.com/aacr/content_public/journal/clincancerres/27/11/10.1158_1078-0432.ccr-20-3703/3/m_2989fig2.jpeg?Expires=1728471578&Signature=DMdtz6wOkGPd9Gi-2AamkpqagGzj~QFCBcJrn5kmXj~HKPvxU3Kj681eW8VNKO4VblK2VaHbb9JpPhsZlk39xO5p84cCLuFoPmZouWC2QLSSR61306LNcAekSjUhubJoPdHB1D3Wu9imM9~fUUv8u9uNKueggGCELY6lkAzE6j-OM~se26FAGn4ksHLTViBoe~9qA80pUK75w237n5AVA3aQfzPJ3PpGDJgnJg~IZfmU3wZA6F0KFxQAGIPdMUELvxg-7e6nRzSdkpzd2~NZTP3FRRu8aen8zz6xWmCd4IMg7Nzrf1HEScrgAyPokH6fOASwPLy794r9Yv9uzjsOQQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA) imaging as contrast recovery, sensitivity, and spatial resolution are far superior for PET imaging. Therefore, some of the smaller lesions seen on 68Ga-DOTATATE MIP may not be visible on planar images of 123I-MIBG scintigraphy, despite adequate MIBG uptake. This should not be confused for greater uptake or a higher likelihood of response to therapy. 124I-MIBG 18F-FDA and 18F-MFBG for PET that are under development should help simplify the comparison between MIBG and SSTRI scans in a given patient." />
imaging as contrast recovery, sensitivity, and spatial resolution are far superior for PET imaging. Therefore, some of the smaller lesions seen on 68Ga-DOTATATE MIP may not be visible on planar images of 123I-MIBG scintigraphy, despite adequate MIBG uptake. This should not be confused for greater uptake or a higher likelihood of response to therapy. 124I-MIBG 18F-FDA and 18F-MFBG for PET that are under development should help simplify the comparison between MIBG and SSTRI scans in a given patient." />
Selection of HSA- 131 I-MIBG versus PRRT for metastatic pheochromocytoma/paraganglioma based on expression of somatostatin receptor and norepinephrine transporter. A, Superior detection of tumors by norepinephrine transporter imaging by 123 I-MIBG (anterior and posterior planar images on the right) compared with SSTRI by 68 Ga-DOTATATE PET/CT [maximum intensity projection (MIP) image on the left] in a 64-year-old man revealing a recurrent tumor in the left adrenalectomy bed along with retroperitoneal lesions, left supraclavicular lymph node, and multiple scattered bony metastatic disease, including cervical bone metastasis. B, Superior detection of tumors by 68 Ga-DOTATATE PET/CT (MIP image on the left) compared with 123 I-MIBG (anterior and posterior planar images on the right) in a 33-year-old woman revealing an extensive recurrent tumor in the right adrenalectomy bed at the level of right mid kidney along with metastatic disease in both lungs, scattered bone metastases in vertebral bodies, axial, and proximal appendicular skeleton. The planar images of 123 I-MIBG only reveal mild uptake of recurrent tumor in the right adrenalectomy bed. C, Similar pattern of tumor detection by both 68 Ga-DOTATATE PET/CT (MIP image on the left) and 123 I-MIBG (anterior and posterior planar images on the right) in a 27-year-old female patient revealing metastatic liver lesions and multiple scattered bony metastatic disease. While interpreting the scans, it is critical to account for the inherent differences between single-photon emission imaging ( 123 I-MIBG scintigraphy) and PET ( 68 Ga-DOTATATE) imaging as contrast recovery, sensitivity, and spatial resolution are far superior for PET imaging. Therefore, some of the smaller lesions seen on 68 Ga-DOTATATE MIP may not be visible on planar images of 123 I-MIBG scintigraphy, despite adequate MIBG uptake. This should not be confused for greater uptake or a higher likelihood of response to therapy. 124 I-MIBG 18 F-FDA and 18 F-MFBG for PET that are under development should help simplify the comparison between MIBG and SSTRI scans in a given patient.
In such a scenario, where the imaging results of 123 I-MIBG and SSTRI scans allow TRT with either agent, the next step is to carefully consider the toxicity profile of each and the patient's characteristics (age, marrow reserve, renal function, prior chemotherapy with alkylating agents or radiotherapies, and location and size of tumors). The most important factors to consider are bone marrow reserve and potential for acute catecholamine/hypertensive crisis. HSA- 131 I-MIBG should be considered in patients with good bone marrow reserve [young patients, no history of prior extended radiotherapies to the bone marrow (spine or pelvis), and fewer bone metastases], whereas 177 Lu-DOTATATE should be considered in patients with more marginal marrow reserve. Another important step is to evaluate cardiovascular status (electrocardiogram and echocardiogram) of these patients, as elevated catecholamines and/or metanephrines can cause cardiac-related adverse events. In patients with elevated catecholamines and/or metanephrines, HSA- 131 I-MIBG might be favored over 177 Lu-DOTATATE, as it is generally not associated with catecholamine crises (Table 1). There is no major preference between HSA- 131 I-MIBG and 177 Lu-DOTATATE in patients with impaired renal function and/or underlying risk factors for nephropathy (diabetes, essential hypertension, older age, and prior nephrotoxic therapies or procedures), although parameters for renal function need to be monitored prior and during follow-up after the administration of both TRTs, and neither of the reagents have been adequately studied in patients with severe renal impairment (30 mL/minute; Table 1). The impact of liver tumor burden on the choice between HSA- 131 I-MIBG and 177 Lu-DOTATATE is equivocal: the median survival was similar for HSA- 131 I-MIBG with or without lung/liver metastases, and baseline liver tumor burden did not have an impact on PFS in phase III NETTER-1 trial of 177 Lu-DOTATATE in GEP-NETs (2, 17). In patients with a lower renal functional reserve, underlying renal disorders, or those with suboptimal bone marrow reserve, dosimetry or low-dose TRT can be used for individualized TRT.
Insurance coverage for selection of imaging modality, as well as TRT is an important consideration. Reimbursement conditions for both MIBG and PRRT vary across, and sometimes within, countries. Currently, in the United States, HSA- 131 I-MIBG is the only FDA-approved radiopharmaceutical specifically for patients with metastatic/inoperable pheochromocytoma/paraganglioma, although 131 I-MIBG therapy has often been reimbursed or supported by third-party payers. 177 Lu-DOTATATE, while approved by the FDA for GEP-NETs, is not approved for treatment of metastatic/inoperable pheochromocytoma/paraganglioma, although National Comprehensive Cancer Network guidelines also include 177 Lu-DOTATATE as an option for this population. There are concerns about the insurance coverage or availability despite the FDA approvals of 123 I-MIBG for the imaging and HSA- 131 I-MIBG in practice, which may vary by region and insurance carrier. Therefore, once the decision for TRT is reached, both 123 I-MIBG and SSTRI should either be performed or the patient should be referred to an institution which has capability of imaging and therapy with these radiopharmaceuticals.
In cases of heterogeneous disease with mismatched MIBG/SSTR avid lesions, the disease coverage may potentially be achieved by combining these therapeutic agents in sequential order, with the first therapy agent being the radiopharmaceutical demonstrating the highest focal uptake in the highest number of lesions (surrogate of total tumor burden; ref. 11), or in a combined regimen (“cocktail”) as demonstrated in a very small prospective cohort (n = 10) of patients (18). However, both approaches have not yet been rigorously tested and should be explored in future. Further, if any progressive lesions lack uptake by both of the above imaging scans, then they can be targeted by additional external beam radiation (11). If there is multifocal non-avid disease, these patients are often better served with other systemic treatment options, most commonly cytotoxic chemotherapy. Additionally, conventional 131 I-MIBG TRT should be considered in cases where HSA- 131 I-MIBG cannot be administered because of logistical reasons. In some jurisdictions, the cost of HSA- 131 I-MIBG is prohibitive in the absence of reimbursement and mandates consideration of conventional 131 I-MIBG.
A special consideration for 90 Y-based PRRT should be made in patients with large-sized tumors, as the maximum emitted energy and path length for 90 Y is greater compared with 177 Lu and 131 I (Table 1; refs. 18, 19). Combinations of 131 I-MIBG and 90 Y-based PRRT are being evaluated to determine whether these can improve targeting of variable-sized tumors and minimize toxicity (NCT03044977). Whether one should precede the other and the optimal combination may be decided on disease burden and avidity on scans.
Recently, PRRT with alpha emitter ( 225 Ac, 213 Bi, 212 Pb, etc.) has emerged and the initial results of a prospective evaluation in 32 patients with metastatic GEP-NETs showed promising results after two cycles with median cumulative activity of 0.84 mCi (range, 0.60–1.2 mCi) of 225 Ac-DOTATATE (20). These patients were either stable after completion of 177 Lu-DOTATATE (n = 14) or progressive on prior 177 Lu-DOTATATE (n = 18) therapy (20). The interim RECIST 1.1 analysis was available for 24 of 32 patients (n = 12, progressive and n = 12, stable after 177 Lu-DOTATATE) 8 weeks after the second cycle of 225 Ac-DOTATATE, and demonstrated an overall PR of 62.5% [15/24; 58.3% (7/12) in progressive cohort], MR of 25% [6/24; 16.7% (2/12) in progressive cohort], and SD of 12.5% [3/24; 25% (3/12) in progressive cohort], respectively (20). None of the patients showed grade 3/4 toxicity, progression of disease, or death within the median follow-up duration of 8 months (20). Furthermore, in another retrospective study of 177 Lu-DOTATATE therapy in 15 patients with metastatic/inoperable pheochromocytoma/paraganglioma, 225 Ac-based PRRT (n = 2 patients) and 131 I-MIBG (n = 1 patient) was administered on a compassionate basis to patients who progressed after three cycles of 177 Lu-DOTATATE, while the remaining patients completed six cycles of 177 Lu-DOTATATE (21). It is important to note that 177 Lu-DOTATATE remains the only PRRT approved for treatment of NETs, and that 90 Y-, 225 Ac-, and other alpha particle–based PRRTs are only available on clinical trials or compassionate use protocols.
Newer radiolabeled SSTR antagonists, such as 177 Lu-satoreotide tetraxetan ( 177 Lu-OPS201), are also undergoing evaluation in NETs, including metastatic pheochromocytoma/paraganglioma (NCT02592707). It is still unclear whether the superior SSTR binding of antagonist drugs will result in improved therapeutic index compared with somatostatin analog–based PRRT.
The clinical decision-making in the selection of patients for appropriate TRT should be personalized. Because of lack of controlled studies, we recommend a pragmatic approach based on expert consensus and opinion that is primarily based on the imaging results of MIBG and SSTRI scans. The agent with the highest uptake should be prioritized while considering the unique toxicity profiles and relevant risk factors (age, marrow reserve, renal function, prior chemotherapy with alkylating agents or radiotherapies, and location and size of tumors). In addition, practical aspects related to availability, insurance, and experience can influence the selection. Finally, multicentric randomized control trials comparing PRRT and HSA- 131 I-MIBG therapy in patients with progressive metastatic/inoperable pheochromocytoma/paraganglioma should help to unravel this conundrum.
J.A. Carrasquillo reports grants from Memorial Sloan Kettering Cancer Center during the conduct of the study. D.A. Pryma reports grants and personal fees from Progenics during the conduct of the study. D.A. Pryma also reports grants and personal fees from Siemens, 511 Pharma, and Fusion Pharma; personal fees from Ipsen and Bayer; and grants from Nordic Nanovector and Lantheus outside the submitted work. W.W. de Herder reports grants from Ipsen outside the submitted work. J. Crona reports personal fees from Novartis and NET Connect during the conduct of the study. J.S. Dillon reports other from Progenics outside the submitted work. T.A. Hope reports research grant from Clovis Oncology, consultant with Curium and ITMa, and advisory board membership with Blue Earth Diagnostics and Ipsen. A.H. Iagaru reports grants from GE Healthcare and Advanced Accelerator Applications, and nonfinancial support from Progenics Pharmaceuticals outside the submitted work. R.J. Hicks reports other from Telix Pharmaceuticals outside the submitted work. J.R. Strosberg reports personal fees from Novartis during the conduct of the study. N. Pandit-Taskar reports personal fees from Progenics during the conduct of the study. There is no disclosure or conflict of interest, employment with NIH, or received money from U.S. Government to conduct research. No disclosures were reported by the other authors.
This work was supported, in part, by the Intramural Research Program of the NIH, Eunice Kennedy Shriver National Institute of Child Health and Human Development (grant no., Z1AHD008735), and was supported, in part, by the NIH, NCI Center Support grant P30 CA008748.